Why Are Dense Breasts Stigmatized?
Leave a Comment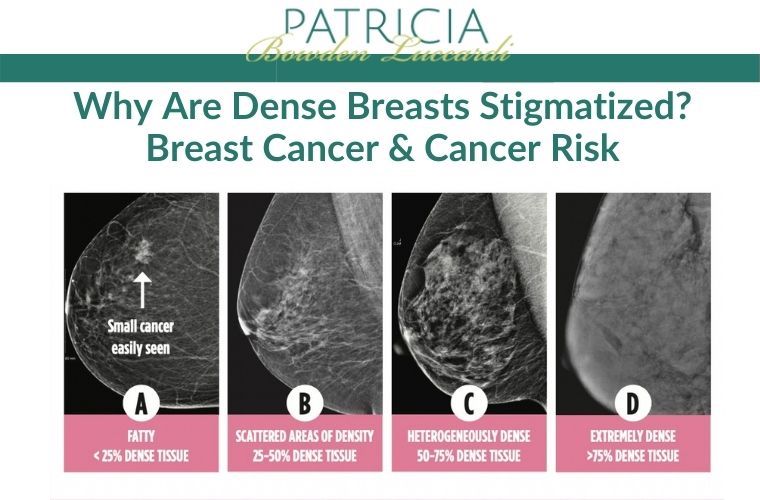
by Anthony Piana, DC, FPACT

The mammogram industry has created a view towards dense breasts that is rather demeaning, as if having dense breasts is similar to a disease. The truth of the matter is, dense breasts are perfectly healthy and normal.
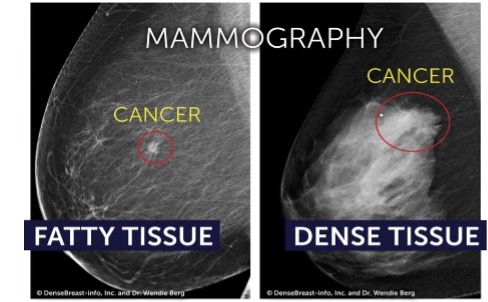
The reason dense breasts have been stigmatized is because mammograms have a difficult time identifying tumors within higher density breasts. This could be caused by the breast being as dense as the tumor, making it hard to distinguish. A way of understanding this is if you were taking an X-Ray of an ice cube that was frozen in a slab of ice. This would cause it to appear no different than the rest of the surrounding area, because the density is the same.
Standards for mammograms have been specifically created around this idea that dense breasts are a nuisance or disease. This is why a few years ago the age recommendation for a mammogram was increased to the age of 50, based on the idea that breast density lowers with age. Still, many women in their 50s have dense breasts.
Another issue is that research studies related to the accuracy of mammograms have adjusted their research perimeters to not include women with dense breasts, despite them being over half of the population. The findings of the studies have shown greater results for mammogram screening, but ultimately they do not reflect well for the general population when identifying tumors.
This isn’t to say that other tests are perfect, though. As an example, thermography has similar limitations when it comes to breast size, obesity, and breast implants. This is why it is important to discuss information with your clients, so they understand that a combination of tests provide the best results — especially when dealing with dense breasts.
Breast Density and Cancer Risk
by Kimberly Lavoie, ACNP-BC, CCRN, SCRN

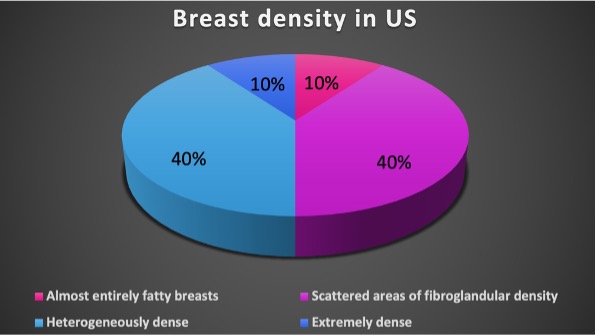
Medical literature is often misleading when describing the impact of breast density on cancer risk. Many studies illustrate the risk probability by comparing women in the 10% highest density category (extremely dense) with 10% in the lowest density category (almost entirely fatty breasts). Comparisons such as these are not statistically meaningful to the remaining 80% of women in the middle, nor should risk comparisons be related to such a small subset population.
More on Dense Breasts
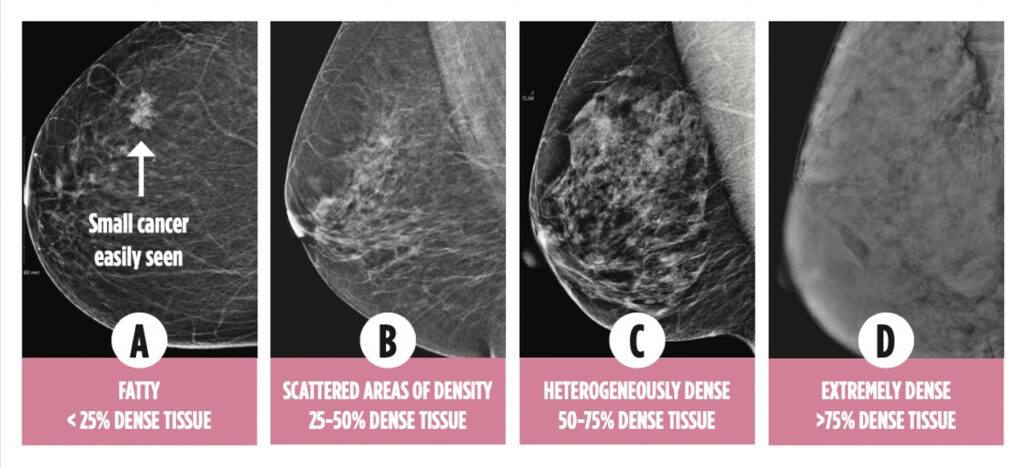
Dense breast tissue is a common finding and is not abnormal. Statistics have shown that approximately 50% of women have dense or highly dense breasts.
However, mammography imaging can make it difficult to detect cancer in women with breast densities. Consequently, mammography is less sensitive in women with dense breasts — that is, it is more likely to MISS cancer. This is precisely why Dense Breast Notification Laws have been implemented.
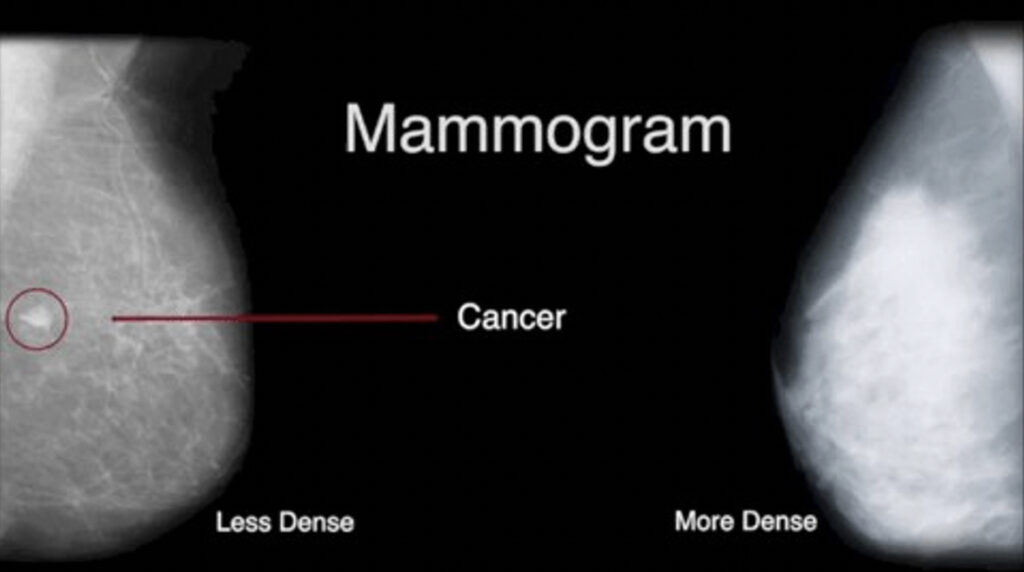
False-negative mammograms result in about 1 in 8 missed cases of breast cancer whereas as false-positive findings can result in over-diagnosis. Over-diagnosing can lead to additional diagnostic testing, invasive procedures, and over-treatment.
According to the American Cancer Society, about 50% of women getting annual mammograms will receive a false-positive finding over a 10-year period. The probability of false-positive findings is even higher when comparison imaging is not available. More than ever we need to continue to educate and help spread THERMOGRAPHIC AWARENESS !!!
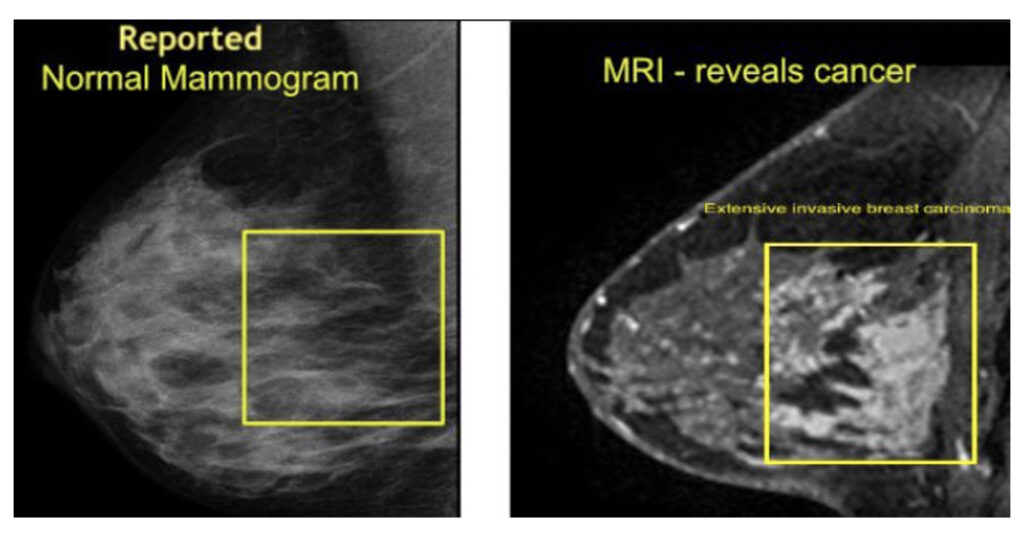
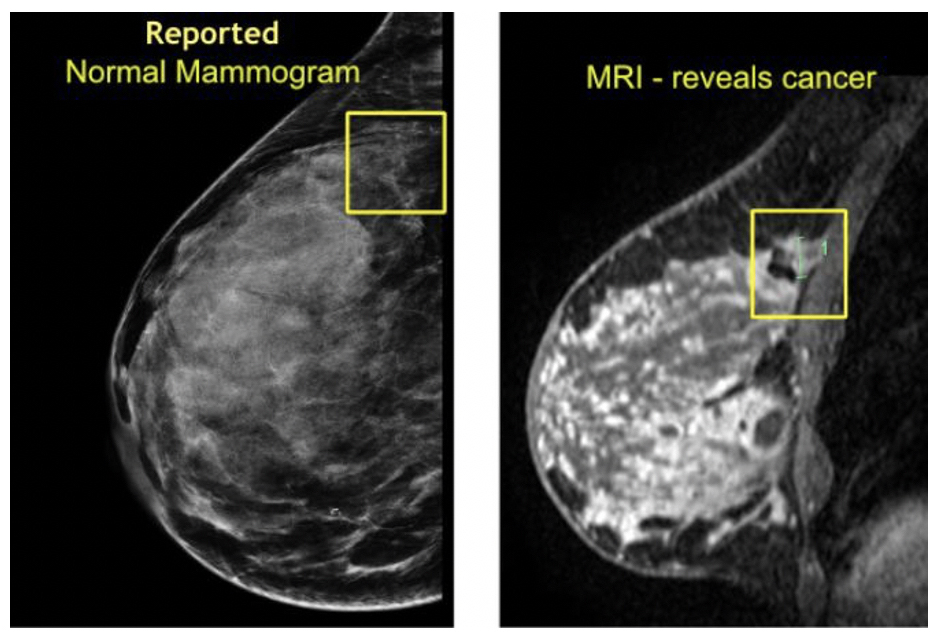
MORE examples of mammograms that were reported as “normal” and less than one week later, MRI reveals “CANCER”
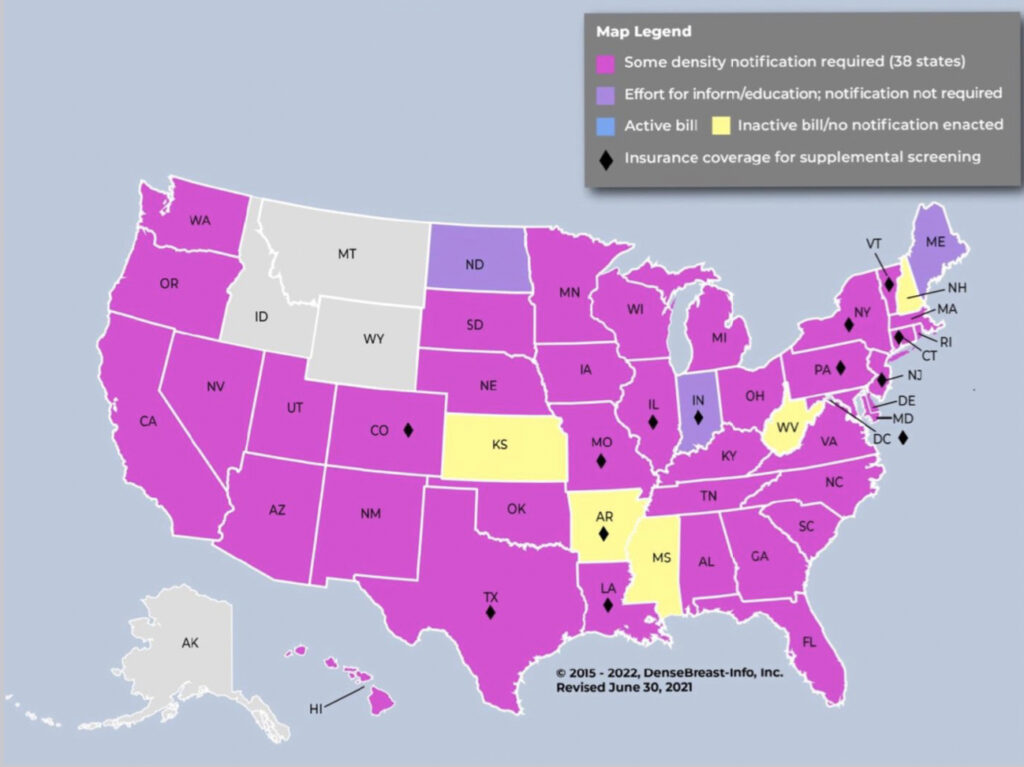
Has your state implemented Dense Breast Notification Laws?
Currently, 38 states and the District of Columbia have enacted dense breast notification laws mandating radiologists to include language in their reports informing women of risks related to dense breasts. If you live in a state that does not have a dense breast notification laws, I encourage you to reach out to your local representative today and let your voice be heard.